How Vein Disease Drives Chronic Inflammation 🔥
Chronic inflammation in the lower extremities is often more than a simple discomfort it is a direct consequence of impaired venous function. When veins fail to efficiently return blood to the heart, pressure within the venous system increases, triggering a cascade of physiological reactions that perpetuate tissue stress. Over time, persistent inflammation can damage the delicate microvascular structures responsible for nutrient delivery and waste removal, creating a self-sustaining cycle that complicates recovery from even minor injuries.
🌡️ Physiology Behind Inflammatory Responses
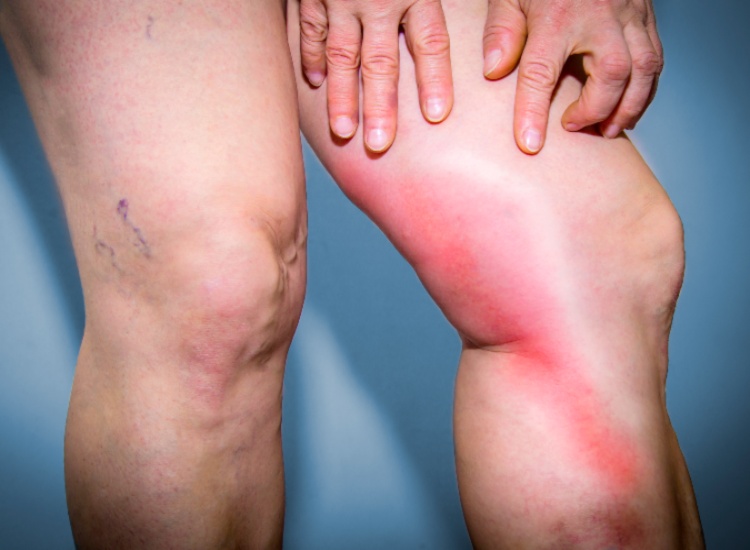
Poor venous circulation causes blood to pool in the lower legs, increasing hydrostatic pressure and stretching vein walls. This mechanical strain signals the release of pro-inflammatory molecules, attracting immune cells to the affected area. While acute inflammation is protective, chronic exposure leads to tissue remodeling, fibrosis, and weakened vessel integrity. Patients may notice swelling, tightness, or a feeling of heaviness in their limbs early signs that vein disease inflammation is advancing. Recurrent episodes of discomfort or tenderness in the lower limbs are common, often intensifying after long periods of standing or inactivity.
🩸 Impaired Oxygenation and Nutrient Delivery
Efficient blood flow is critical for tissue repair. When veins underperform, oxygen delivery diminishes, and metabolic waste accumulates in the interstitial space. This environment slows the healing process, leaving minor injuries at higher risk of becoming persistent or complicated. The cumulative effect of reduced oxygenation and ongoing inflammatory signaling contributes not only to swelling and discomfort but also to structural changes in skin and subcutaneous tissue.
💡 Visible Signs and Skin Changes
Chronic inflammation often manifests visibly as skin discoloration, thickening, or increased sensitivity. Patients may observe reddish-brown patches, shiny or taut skin, and areas prone to bruising with minimal trauma. These changes indicate that inflammatory mediators have begun altering connective tissue and dermal integrity. In more advanced cases, skin may feel firm or hardened, signaling that the inflammatory process has become entrenched and long-term tissue remodeling is underway.
📝 Key Indicators Patients Should Monitor:
- 🦶 Swelling in the ankles or lower legs, especially after standing
- 💤 Persistent heaviness or fatigue in the legs
- 🎨 Reddish-brown discoloration or shiny, tight skin
- 🤕 Tenderness or recurrent minor bruising
- 🚶 Increased episodes of leg pain during activity
Monitoring these signs allows patients to seek timely evaluation by a vein specialist. Early recognition of vein disease inflammation can prevent progression to severe complications and preserve both skin and vein health.
⚙️ Breaking the Cycle with Targeted Intervention
Addressing the underlying venous insufficiency is critical to halting chronic inflammatory cycles. Interventions may include compression therapy, minimally invasive vein procedures, and lifestyle strategies aimed at improving venous return. Elevation of the legs, structured physical activity, and careful skin care support tissue recovery. By restoring more effective circulation, inflammatory signaling diminishes, oxygenation improves, and tissue repair mechanisms regain efficiency. Proper coordination and expert guidance help ensure both minor and persistent vein issues are managed effectively, reducing long-term risk.
🧪 Long-Term Effects of Unchecked Inflammation
If left unmanaged, chronic inflammatory processes can contribute to vein wall remodeling, fibrosis, and an increased likelihood of venous ulcers. Tissue changes may become irreversible, complicating wound healing and increasing susceptibility to infection. Chronic swelling can also exacerbate discomfort and limit mobility, creating a negative feedback loop where inactivity further impairs circulation. These long-term effects underscore the importance of proactive monitoring and timely intervention by qualified vascular specialists.
🌿 Lifestyle Considerations for Supporting Vein Health
While medical evaluation is essential, patients can complement professional care with supportive strategies: maintaining a balanced diet to reduce systemic inflammation, staying hydrated to improve blood viscosity, and avoiding prolonged periods of immobility. Protective measures, such as using appropriate footwear, elevating legs periodically, and wearing compression garments when recommended, further aid in reducing venous pressure and supporting tissue repair. Simple, consistent practices help stabilize circulation, lessen inflammation, and mitigate leg pain over time.
💠 Role of Specialized Care
Chronic inflammation veins require careful oversight by experienced professionals who can tailor treatment plans to the severity of the condition. A vein specialist in Palm Desert provides comprehensive evaluation, incorporating imaging studies and clinical assessment to map vein health, identify reflux points, and guide intervention. Collaborative care involving both patient engagement and expert management is the most effective way to break the cycle of inflammation, restore proper circulation, and preserve long-term leg function.
Persistent inflammation signals a complex interaction between vein health and tissue response. By observing early indicators, implementing supportive measures, and working closely with vascular specialists, patients can limit the impact of chronic inflammation, protect skin integrity, and reduce the risk of long-term complications associated with impaired venous circulation.

Andy Sharify
The founder and owner of The Vein Institute of the Desert. He oversees the clinic, ensuring exceptional service and a patient-focused approach to vein care. Andy is dedicated to creating a comfortable and supportive environment for every patient.
