What is Lipodermatosclerosis ⚠️
Lipodermatosclerosis is a condition that signals advanced vein problems and is often misunderstood. This form of skin and tissue change occurs when long-standing venous dysfunction causes prolonged pressure in the lower legs. Over time, inadequate blood flow triggers inflammation and fibrosis, leading to hardening of the skin, tenderness, and noticeable discoloration. Patients may initially overlook subtle signs, but early recognition is essential for managing progression and protecting long-term leg health.
🌡️ How Chronic Venous Insufficiency Contributes
In individuals with impaired venous circulation, blood can accumulate in the lower legs, increasing pressure within the veins. This inefficiency reduces the veins’ ability to return blood effectively to the heart, leading to fluid and red blood cell leakage into surrounding tissues. Over time, iron from these cells deposits in the skin, causing pigmentation changes and contributing to a firm, tight texture in the lower legs. Vein specialists frequently observe this combination of swelling, skin hardening, and discomfort in patients with advanced vein conditions.
🩸 Early Tissue Changes and Inflammation
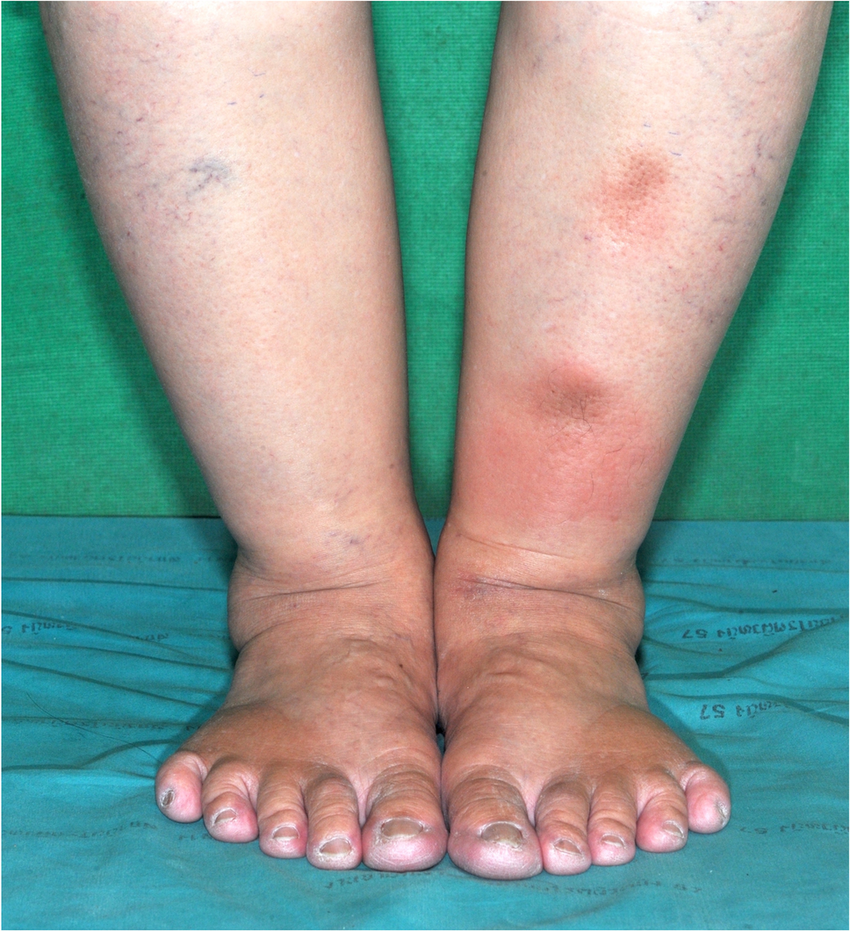
The initial stage of this vein-related skin condition is marked by subtle inflammation around the ankles or lower calves. Skin may appear reddish or slightly purple, and mild swelling can occur after prolonged standing. Many patients report heaviness or aching in the legs, often dismissing it as fatigue or age-related discomfort. At this point, timely intervention can prevent further fibrosis and protect tissue integrity. Chronic irritation without treatment accelerates skin thickening and reduces elasticity, making daily movement more uncomfortable.
🎨 Visible Skin Alterations and Leg Tightness
As the condition progresses, skin tightening in the legs becomes more pronounced. The surface may feel firm or “woody,” particularly along the medial aspect of the lower leg. Discoloration deepens into brownish or purplish hues, reflecting iron deposits and chronic inflammation. In some cases, small patches of atrophie blanche—white, scar-like areas appear, indicating localized tissue damage. These visible changes are not only cosmetic; they signal that the underlying veins are struggling to manage blood flow, increasing the risk of venous ulcers if untreated.
🔍 Signs to Watch for in Advanced Stages
Recognizing this advanced vein-related condition early can make a significant difference. Key indicators include:
- 🦵 Firm, hardened areas of skin: Often painful to touch and may limit mobility.
- 🎨 Persistent discoloration: Reddish-brown or purplish patches that do not fade after rest.
- 💧 Swelling and fluid retention: Legs may swell noticeably after standing, reflecting ongoing venous pressure.
- ⚡ Skin sensitivity: Tenderness, itching, or burning sensations, sometimes accompanied by flare-ups of inflammation.
These symptoms collectively highlight the importance of monitoring advanced venous disease and consulting a qualified vein specialist when noticeable changes appear.
🧪 The Mechanism Behind Fibrosis
Repeated venous hypertension triggers an inflammatory response in subcutaneous tissues. Fibroblasts are activated to repair tissue damage, but overactivity leads to fibrosis. This process thickens the skin and reduces its elasticity, causing discomfort and contributing to skin tightening in the legs. The longer venous reflux and pressure remain untreated, the more pronounced these structural changes become. Early detection and intervention can slow or even partially reverse fibrosis, emphasizing why routine monitoring is crucial in high-risk patients.
⚠️ Long-Term Implications Without Intervention
If this advanced vein condition is overlooked, the consequences go beyond cosmetic issues. Chronic inflammation and tissue fibrosis can lead to noticeable skin tightening in the legs, increasing the risk of venous ulcers, infections, and lasting tissue damage. Leg mobility may become limited due to stiffness, and ongoing discomfort often impacts overall quality of life. Prompt evaluation by a vein specialist helps ensure patients receive proper care to manage swelling, address venous reflux, and preserve skin and tissue health before serious complications develop.
🏥 Why Professional Evaluation Matters
The Vein Clinic in Palm Desert highlights that lipodermatosclerosis is a warning sign, not an isolated skin condition. Medical evaluation can determine the severity of venous reflux, assess tissue health, and guide interventions such as compression therapy, lifestyle modifications, or procedural treatments. By addressing the root cause chronic venous insufficiency patients can reduce progression, prevent ulcers, and maintain leg functionality. Awareness of early indicators, combined with expert care, significantly improves outcomes in vein health.
💡 Recognizing the Silent Progression
Many patients fail to act until discomfort or visible changes become pronounced. Recognizing subtle early signs such as mild swelling, skin tightness, and minor discoloration can prevent the condition from advancing to severe stages. Regular observation, timely consultation with vein experts, and adopting preventive measures form a critical strategy for long-term leg health. This type of advanced vein-related skin change serves as a clear signal that veins are under stress and require medical attention to prevent chronic complications.

Andy Sharify
The founder and owner of The Vein Institute of the Desert. He oversees the clinic, ensuring exceptional service and a patient-focused approach to vein care. Andy is dedicated to creating a comfortable and supportive environment for every patient.